School nurses are part of the multi-disciplinary team that are required to attend child protection case conferences. As part of this process, school nurses undertake a health assessment and report on the findings. Child protection conferences can be up to 2 hours long and school nurses are often required to reattend at 3 months and, if the child protection plan continues, 6-monthly until the child or young person (from here on in referred to as client) are considered not to be at risk of serious harm. The impact of the amount of time school nurses spend in this arena on the public health service delivery has been the subject of much debate (Children's Commissioner, 2016a).
The Nursing and Midwifery Council (NMC, 2004) remarked that health assessment is a key component of public health nursing practice. In practice, specialist community public health nurses and school nurses need to gain a complete picture of a client's individual life and circumstances in the search of their health needs. A health assessment should collect data about the normal abilities of the client, risk factors that may result in health problems, and any changes in the client's health to get a clear overview of the health status of the client. It also gives an opportunity to encourage healthy habits, prevent potential health problems, and manage current health problems efficiently (Weber and Kelley, 2021).
‘Co-production is a key element of this health assessment, which allows the joint effort of a school nurse and client to complete what is required in a reciprocal manner.’
A safeguarding colleague and I were selected to work on a scoping exercise with the trust's public health nurse consultant to investigate school nurse health assessments nationally. This scoping exercise found a paucity of research that critiques and evaluates school nurses' health assessments, and while school nurses in practice often adopt their own models, few are published.
It could be argued that if school nurses have concluded from a health assessment that a client has a specific health need and is being supported by a specialist service or an appropriate referral has been made, the practitioner from the service in question may be better suited to speak about that health need in a review child protection conference (RCPC). This would free up time for school nurses to improve the health and wellbeing of clients. To be clear, this is not the school nurse absolving their safeguarding responsibility, safeguarding runs through the core of all their work. This is about the school nurse seeking and supporting health needs and ensuring the correct person is present in the RCPC to speak to any health needs (e.g. the diabetes clinical nurse specialist who is supporting the client with diabetes). These practitioners are best placed to offer first-hand updates and identify family strengths. Another advantage would be, for example, that if a client being supported by a child protection plan with diabetes was not brought to their appointment, the diabetes clinical nurse specialist knowing who the social worker is would liaise directly with them to share this information. This way, a contemporaneous and first-hand picture of the lived experience of the client is captured.
School nurses would remain part of the professional network by conducting a health assessment, sharing its findings, gaining consent to receive minutes, and by ensuring the client is brought to safeguarding supervision.
This is where a holistic standardised health assessment comes in to provide that confidence for the school nurse but also to ensure that information is shared. This case study shows the journey of the development of a health assessment for clients being supported by a child protection plan that captures the voice of the child or young person while providing evidence to support the decision of the school nurse to safely not attend an RCPC. Central London Community Healthcare NHS Trust (CLCH) has allowed me to explore this nationally debated topic and to look into a potential solution.
Why the need for change
Recognising these time concerns, the Children's Commissioner for England (2016b) commissioned a Lightning Review, which examined the possible weaknesses in local systems that could impact school nurses' ability to perform their duties. It highlights the Commissioner's concerns that school nurses are spending more time on bureaucratic child protection duties and paperwork than on their duties of improving the health and wellbeing of clients. We are all aware that we spend 2–3 hours in a case conference and often contribute very little.
On the back of this CLCH children's safeguarding team internally audited school nurse involvement from two boroughs child protection procedures – the numbers in Table 1 speak for themselves. The publication of a recent report suggests that there are only 2 000 school nurses nationally (Hunter, 2023); therefore it is likely that school nurses nationally are spending more than 70 hours per month on child protection caseloads. Something needs to change. We need to be bold and inventive.
Table 1. Minimum time spent per child subject to a CP plan
| Activity | Hours spent | Number per year | Total hours |
|---|---|---|---|
| Attendance at case conference | 3 | 3 | 9 |
| Core groups | 2.5 | 8 | 20 |
| Report writing | 1 | 3 | 3 |
| Health assessments including documentation/arranging etc | 3 | 3 | 9 |
| Communication with family | 3 | 3 | 9 |
| Safeguarding supervision | 2 | 1 | 1 |
| Liaison with professionals | 3 | 3 | 9 |
Notes: An average CP caseload for a school nurse is 14, this equates to 70 hours per month per school
Table reproduced with kind permission of the audit author
The bold and the inventive
CLCH is a pan-London community NHS trust covering 11 boroughs. It provides community healthcare services for more than two million adults and children across London and Hertfordshire and is as diverse and dynamic as the population it serves.
In 2022, at the instigation of our chief nurse, our public health nurse consultant brought school nurses together to combine best practice. The Time to Shine project was born to standardise, modify and amplify the voice of school nurses in CLCH. Five working groups were developed including a safeguarding working group. Chaired by the associate director for safeguarding, the aim was to consider current safeguarding practice and the confidence of the school nursing service to champion their role and the voice of children across the safeguarding system. The Lightning Review (Children's Commissioner for England, 2016b) evidenced the need for change and helped frame three objectives:
- To evaluate the role of school nurses when there are safeguarding concerns about the risk and vulnerability of a child or young person
- To review the process regarding the school nursing service attendance at initial and review case conferences
- To explore the implementation of a CLCH/standardised health assessment to support decision-making/care planning.
What should a health review capture?
Each child coming to conference will have unique needs and vulnerabilities. School nurses need to search for, discern, document, and share health needs.
Following the scoping exercise, the ensuing discussion concluded that a health assessment should promote engagement and discussion. It should be a joint venture done with the client, not done to the client, in a confidential setting. This engagement should be non-distressing and enjoyable and beneficial for both, ensuring the nurse makes that contact matter. These thoughts echoed the evidence base offered in key documents such as those published by the Department for Health (2012) and the British Youth Council (2011), and the skill set required by school nurses (NMC, 2022).
A client is more than a physical entity, they are an emotional entity too, and if applicable, they are also a sexual being. All of which we can capture in a health assessment and offer public health support and perspectives on, and if necessary, we can signpost onto, more specialised colleagues or liaise with parents and the school team.
As highly trained public health practitioners, frequently dual registered and having studied at degree level or higher, school nurses can use the results of this health assessment to predict risk and intervene early to benefit our clients.
Bioecological thinking
A client is not just an individual, they are also a family member, a pupil, a member of a faith, a friend, a patient, a member of a community, football team, drama group, all these things or just some of these things. While we embrace individuality, we should not see a client as just the person sitting in front of us.
We have likely all heard the phrase it takes a village to raise a child. Bronfenbrenner (1999) developed the bioecological model after recognising that the individual was overlooked in other theories of human development, which were largely focused on the context of development. The framework emphasizes the importance of understanding bidirectional influences between individuals' development and their surrounding environmental contexts. Bronfenbrenner suggested that individuals constantly interact with these systems. He also stated that both individuals and their environments constantly affect one another. Simply put, Bronfenbrenner captures the village raising the child and how the child and village interact and affect one another.
The health assessment recognises this and that is why contextual, educational, and familial information is gathered and is so important.
A modern-day school nurse assessment
Co-production is a key element of this health assessment, which allows the joint effort of a school nurse and client to complete what is required in a reciprocal manner (NHS England, 2023). The assessment is multifaceted and has the voice of the client running through it. Gradually different areas of the client's life are discussed and together make a robust, thoughtful, and holistic piece of work that grows and ebbs, guided by a school nurse. The school nurse is the conductor of this assessment by building on the uniqueness of the client; they learn more about them by asking open questions to encourage a client's voice to be heard and actively listen. This way, a comprehensive collaborative health assessment is achieved.
As you can see in Table 2, the assessment is split into various sections so that it is easy to offer choice to the client as to where they want to start.
Table 2. The model of assessment
| Primary assessment | Secondary assessment |
|---|---|
| Confidentiality | Confidentiality |
| All about me and what I can do | All about me |
| My home and community | My home and community |
| My physical wellbeing | My physical wellbeing |
| My education and hopes | My education or training and hopes |
| My emotional wellbeing and wishes | My emotional wellbeing and wishes |
| Consent and feedback | My Sexual wellbeing |
| Substance Misuse | |
| Consent and feedback |
This health assessment differs to those used presently as not only does it ensure the client's whole world is captured, it also uses resources that allow public health messages to be discussed and enables school nurses to offer support. Examples of this include discussing the Eat Well Plate, immunisations, and sexual wellbeing. Another difference is that it includes the opportunity for school nurses to discuss emotional health and assesses this using the evidence-based revised childhood adolescent depression score (RCADS) that can go on to bolster an appropriate referral to specialised services if needed. This is important due to the increased concerns about the mental health of children and young people (NHS Digital, 2022). Figure 1 shows how the assessment has been completed by a client and how the client's voice is captured.
‘…it includes the opportunity for school nurses to discuss emotional health and assesses this using the evidence-based revised childhood adolescent depression score…’
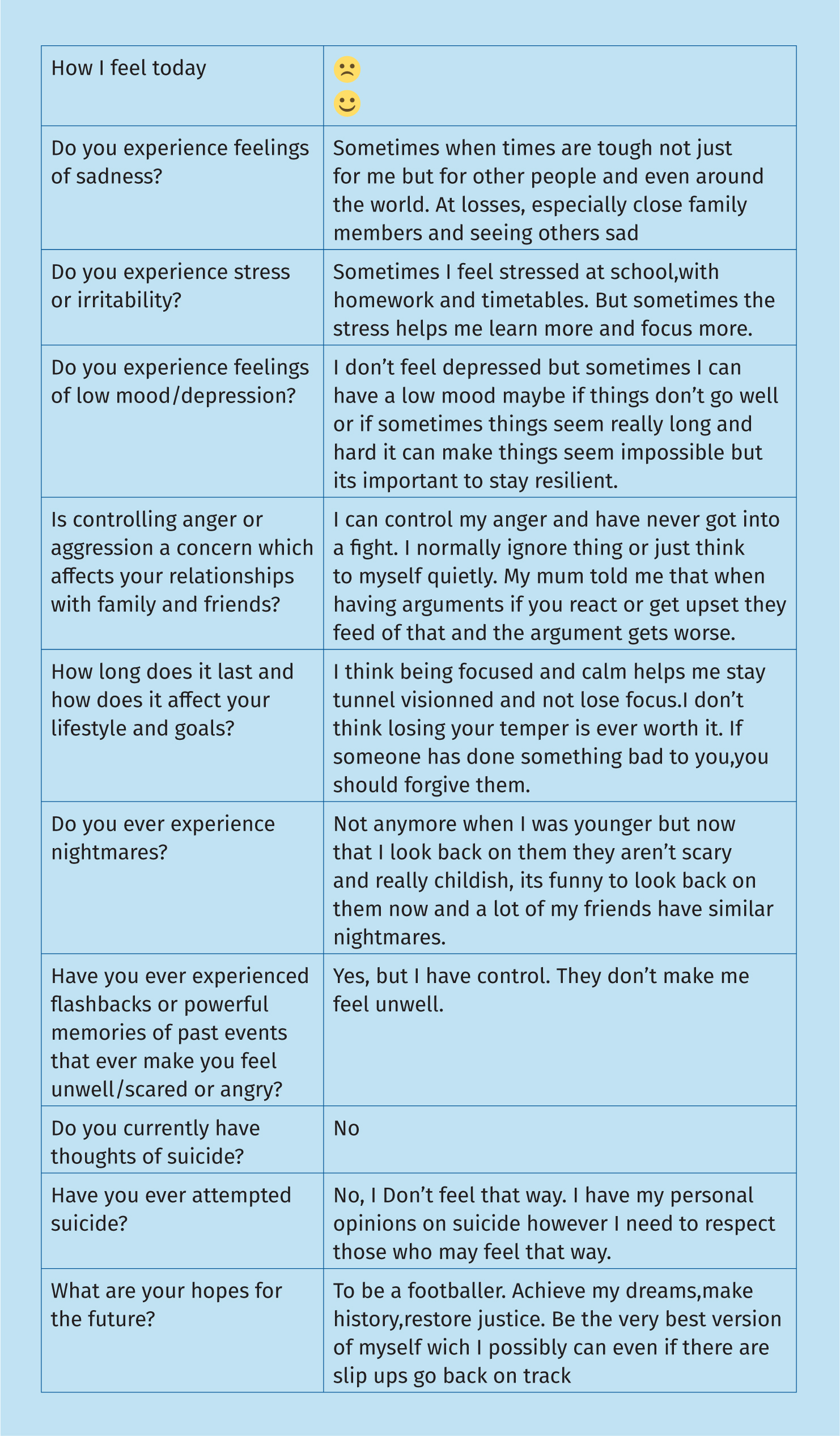
The assessment opens by discussing consent. The client signs to say that we have talked to them about this and more importantly they have understood that although what they say in the room is confidential, there are times this may need to be broken, but we will work in partnership with them to share the information that needs to be shared. In the case of the primary aged assessment, parents would be invited to attend the health review and their consent sought to see their child. The first section is for the client to fill in as much as possible and gathers information about them and their likes and abilities.
In the last section, consent is gained from the client as to whom we can share this assessment with and gather their feedback using the friends and family test (NHS England, 2023). We also gain consent from the client to keep in touch by receiving meeting minutes and seeing them again. Parents/carers would also be consulted, and consent gained to remain part of the professional network.
The Bronfenbrenner model is evident in this health needs assessment by seeking how, if a client has poor mental health, this may impact on peer or familial relationships and educational attainment or if a client is not attaining academically, how this can influence emotional wellbeing and how that person is perceived by peers and potentially family. My hope is that by school nurses becoming familiar with this assessment they will be resourceful and gather the information in a creative, flexible, and enjoyable manner that school nurses are good at. However, as you can see, the health assessment is comprehensive and robust and allows nurses to guide a conversation with the clients if needed. It may look overwhelming, but school nurses have the skills of active listening and asking open questions to capture what the client tells them to complete the assessment. School nurses are also able to support children with special educational needs and disability to capture their voice (NMC, 2022).
School nurses are undertaking this assessment with the client, not doing the assessment to them – they must be involved, it is a collaboration. Ultimately, it should be all about them and very little about the school nurses. However, the time saved by school nurses after doing this assessment and after discussion with their safeguarding supervisor, without attending review case conferences, can most definitely be about school nurses and how they spend this freed up time being in schools, offering training, being visible and accessible to offer confidential support.
School nurses recognising the art of nursing
School nurses are by nature a creative and flexible group of nurses. Florence Nightingale (1946) recognised that nursing is an art. Acheson (1988) also recognised the work of public health as the science and art of preventing disease, prolonging life, and promoting health through the organised efforts of society. This art is what is needed here to ensure the health assessment is done with and not to the client. This may involve creative thinking to ensure that they don't feel that they are being questioned in a formal manner and enable them to build trust and confidence in us. For newer colleagues there are some ideas in Table 3 to begin a health assessment, even though we are all different and the way the assessment is used is up to the practitioner.
Table 3. Ideas to complete the assessment
|
Now for some reassurance
In the emotional wellbeing section, suicidal ideation and self-harm are discussed. A literature review conducted by Dazzi et al (2014) concluded that none of the papers reviewed found a statistically significant increase in suicidal ideation among participants asked about suicidal thoughts. What was found was that asking the question and acknowledging and discussing suicide may be a protective factor. What is important for school nurses is to remain calm, be non-judgemental, actively listen to the client and remember they never work in isolation, so they can seek support and share information.
If necessary, it may be helpful to use Pantosaurus (NSPCC, 2023) with his child-friendly way of conveying the message to keep their bodies private, the importance of telling an adult and the suggestion of the school nurse as a safe person.
The pros and cons
It is a long assessment, but it needs to be to give school nurses confidence that the client has no unmet health needs or is appropriately supported with their health needs. It takes approximately an hour, but RCPCs can be more than 2 hours, so the free time from bureaucratic child protection duties and paperwork (Children's Commissioner for England, 2016a; Munro, 2011) will soon add up.
This assessment model needs to look more child-friendly, which is why there is a community engagement working party within Time to Shine and some young people will help on that front.
It does need school nurses to be confident and be able to ask some sensitive questions and it may require them to access training to support any identified learning need the client may have.
The assessment has lots of room for answers so after it is completed, it is just a matter of uploading the assessment onto the client's records along with a note to say a health assessment has been completed and to see uploaded documents. In the future CLCH will be building a template on the electronic records, so the time spent writing up the contact will diminish.
This assessment is such a good opportunity to utilise skills, build relationships and offer choice, as well as capturing the voice of the child. The positives of using it seem to outweigh the challenges and allow school nurses to be the public health practitioners they are trained to be, delivering key messages to their cohort of clients and empowering them for the future. As well as making every contact count (Varley and Murfin, 2012).
The future
After a successful pilot and changes made, the assessment has been sanctioned for use within the trust and the safeguarding team has implemented it into a new policy and pathway that ensure it is safe and appropriate for a school nurse not to attend an RCPC. This is currently being shared and advocated for use with the commissioner and social care partners. It is anticipated to be rolled out as standardised Trust policy imminently. A training package has also been developped to support the roll out of the health assessment. I look forward to colleagues evaluating its use and gaining feedback from all stakeholders, including young people, with a formal evaluation to follow.
What has been learnt
- You must be bold to make such a change and I never worked in isolation in developing this model. Working with clients and colleagues has been vital and rewarding. This has allowed rich and varied ideas to be merged into a contemporaneous project that allows the voice of the child or young person to flourish.
- School nurses at the frontline of practice are best placed to effect a change that will ultimately benefit the client.
- The time spent thinking deeply about assessment and safeguarding has been interesting and creative, and taps into the art and science of nursing that allows ‘out of the box’ thinking.
- The need to share and advocate wholly for what school nurses do is palpable.
- School nurses are underutilised, sometimes underestimated, highly qualified and knowledgeable professionals who are best placed to be in schools delivering key public health messages to empower and inform the next generation.
- The future is exciting as the model and policy become standardised practice within the trust and school nurses have led the way in researching, writing, and piloting it.
- School nurses are in a privileged and trusted position to build a relationship and gain an insight into a client's life, one to be revered and to be nurtured.


