Internationally, the UK is underperforming in the context of young people's health. Young people in the UK with a long-term condition are more likely to experience a poorer quality of life than those in most comparable countries (The Nuffield Trust, 2019). In 2019, the NHS Long Term Plan (LTP) reported that there were 1.7 million children with longstanding illnesses in England (NHS, 2019). Within the plan there is a focus on improving the quality of care for children with long-term conditions by sharing best clinical practice, quality improvement projects and integrating paediatric skills across services (NHS, 2019).
Compared to other wealthy countries, a greater number of childhood deaths are caused by non-communicable diseases in the UK, although there is uncertainty as to whether this high mortality reflects higher environmental risks in the UK or issues with health care for long-term conditions (Royal College of Paediatrics and Child Health, 2017).
Having a child with a long-term condition has a broad psychosocial impact (Bowes et al, 2009; Nygård and Clancy, 2018). Parents develop expertise in the management of their child's condition, including bridging the gaps in communication within health care (Smith et al, 2015; Willis et al, 2015). Parents report wanting to work with health care to provide the best care for their child, but often find communicating with clinicians stressful (Nygård and Clancy, 2018). ‘Family-centred care’ is important in improving the care provided (Smith et al, 2014). However, there is little research on how parents' and clinicians' views can be integrated to provide care for the child, or what areas of the health-care system require change.
Research has shown a positive association between patient experience, clinical effectiveness and patient safety (Doyle et al, 2013). Parents can provide a uniquely personal insight into the health care provided to their child which can highlight gaps in care or identify areas for improvement (Smith et al, 2015; Smith et al, 2014). This can then result in improvements in health care and better clinical outcomes for young people with long-term conditions.
This research was undertaken in the UK and relates to NHS service provision. The aim is to gain an understanding of parents' experience of and contribution to health care for children with long-term conditions.
Methods
Study design
This qualitative interview study was guided by a phenomenological methodology, to allow exploration of the parents' subjective experiences (Smith et al, 2009). A method of co-production with a stakeholder group was adopted to ensure patient and public involvement (PPI) (INVOLVE, 2012; 2018). The four stakeholders included one voluntary organisation representative, one parent representative and two NHS employees (management and patient advice and liaison service). Semi-structured interviews were conducted using a topic guide derived from a literature review. This was amended in light of suggestions made during the first stakeholder meeting and emergent themes from interviews were incorporated. The researcher was a fourth-year medical student, with no prior relationship to the participants.
Ethics
Ethical approval was granted in accordance with the associated university ethics review procedure, as administered by the medical school. Each parent was provided with an information sheet and consent form. Both were read and signed by the participant before proceeding with the interview.
Sampling and recruitment
Recruitment was through a local parent carer charity, and a volunteer email list of The University of Sheffield staff. Purposive sampling was used to ensure parents fitted the study criteria and to ensure a variation in the long-term conditions represented. This resulted in 10 participants. Snowball sampling via participants was employed to increase participation to 15 parents.
Data collection and analysis
Semi-structured interviews (n=15) took place between February and March 2020. Seven face-to-face interviews and eight via telephone due to the COVID-19 pandemic. Recruitment ceased when data saturation was achieved. The children were not present during the interviews. The interviews ranged from 30 to 75 minutes. Topics included parents' experience of living with a child with a long-term condition, which areas of their lives had been affected, their thoughts on the care their child had received from NHS services and feedback to the NHS about their child's care.
The interviews were audiorecorded and transcribed verbatim by the researcher. All identifying features were removed at this stage. Framework analysis was used to develop themes from the interviews (Gale et al, 2013). Triangulation was ensured by the research team, who coded several interviews for independent verification of the themes (Lincoln and Guba, 1985). The analytic software NVIVO version 12 was used to code and organise the data. The results were presented to the stakeholder group as a form of member checking. Reflective notes were made after each interview, which aided the reflexive journal kept by the researcher.
Results
The participant demographics are displayed in Table 1.
Table 1. Participant demographics
| Px | Parental sex | Age | Relationship status | Employment | Child's long-term condition(s) by specialty | Child's age |
|---|---|---|---|---|---|---|
| 01 | Female | 41 | Married | Part time | RespiratoryGastroenterologyImmunology | 5y |
| 02 | Female | 54 | Married | Full time | Neurology | 15y |
| 03 | Female | 46 | Single | Unemployed, full time carer | Metabolic MedicineNeurology | 15y |
| 04 | Female | 54 | Married | Part time | Rheumatology | 16y |
| 05 | Female | 40 | Living with partner | Part time | Rheumatology | 3y |
| 06 | Female | 36 | Single | Full time | Cystic fibrosis | 4y 11m |
| 07 | Female | 40 | Engaged | Part time (husband full time carer) | Neurology | 3y 11m |
| 08 | Male | 35 | Engaged | Unemployed, full time carer | Neurology | 3y 11m |
| 09 | Male | 42 | Married | Full time (wife full time carer) | NeurologyPsychiatryEndocrinology | 14y |
| 10 | Female | 41 | Married | Part time | Dermatology | 7y |
| 11 | Female | 39 | Living with partner | Part time | RespiratoryCardiologyOrthopaedics | 5y |
| 12 | Female | 39 | Married | Part time | NeurologyGastroenterologyCardiologyRespiratoryPsychiatry | 11y |
| 13 | Female | 48 | Married | Full time | Metabolic medicine | 10y |
| 14 | Female | 37 | Married | Part Time | Endocrinology | 4y 6m |
| 15 | Male | 42 | Engaged | Part time (wife full time carer) | Neurology | 13y |
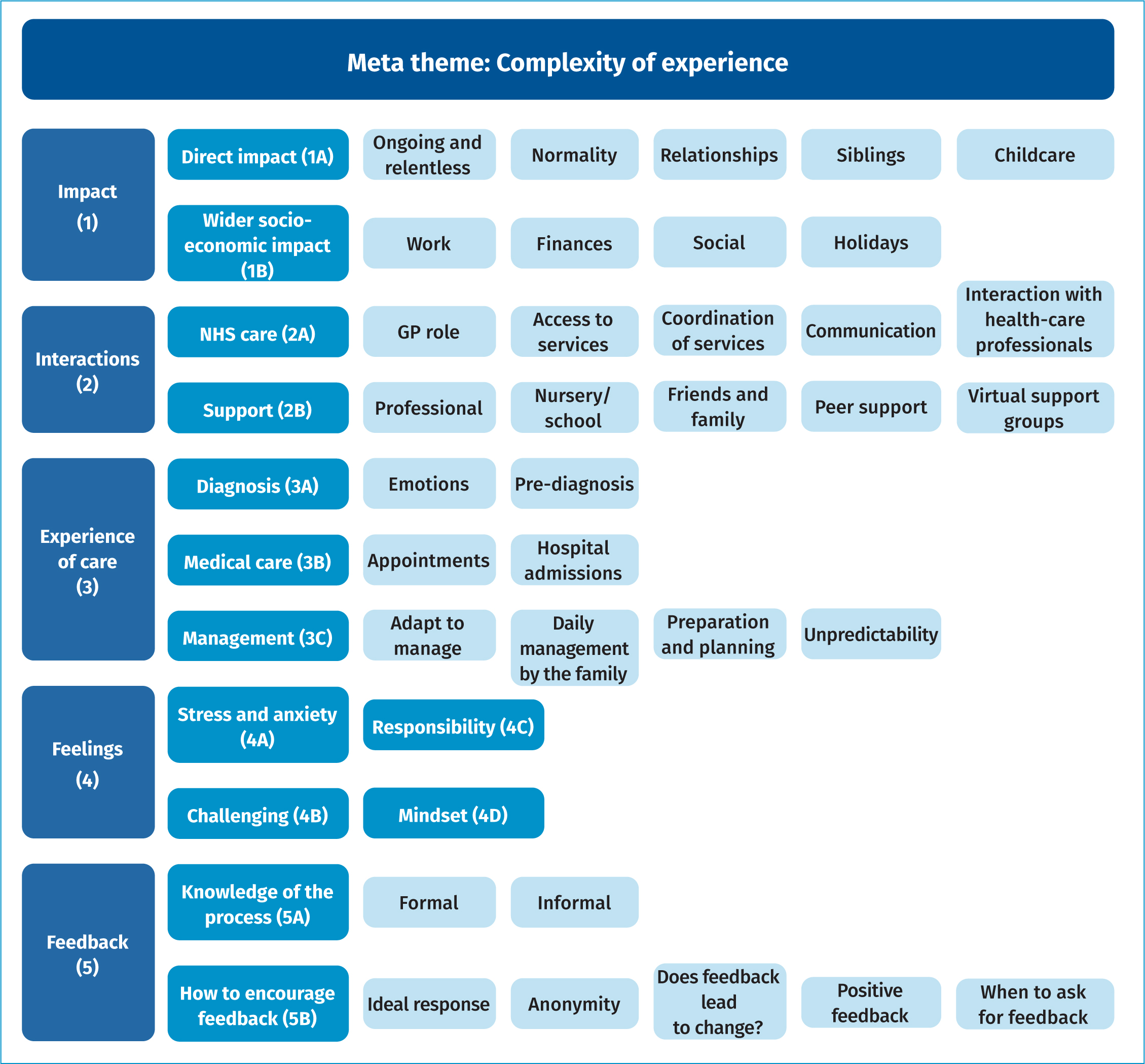
The framework analysis produced five key themes (Figure 1): impact of having a child with a long-term condition, interactions with NHS staff and wider support networks, experience of care from diagnosis through to ongoing management, and feelings and feedback to NHS including formal and informal mechanisms. The focus of this paper will be on the first three themes.
Impact
The results indicate an extensive impact on the lives of parents including emotional, functional, interpersonal, occupational, financial and social impacts. Their experience affected most aspects of their lives.
Parents reported the life-changing, ‘ongoing and relentless’ impact of caring for a child with an long-term condition. The time-consuming management meant there was not as much capacity for ‘family time’.
‘…all the time I feel on a daily basis, really responsible for trying to get the best I can get from him… Or making the best for him and his life in the future.’
P02
The aspiration to normality for the family and child was a common theme. The relationships within the family are altered, due to conflict over management and the requirement for the child with the long-term condition to be the priority.
‘Erm, our daily life basically everything revolves around Holly’
P12
Parents were also very aware of the emotional impact their situation can have on siblings, but found it difficult to balance the competing needs of their children. Work is a very important factor and can be a great source of support when flexibility is offered. A substantial financial impact was reported, as parents were unable to work as much and because of the increased costs associated with their child's condition.
‘It's so expensive to have a child in hospital…for parking, for getting food, for trying to be healthy…’
P01
These findings indicate the immersive experience of caring for a child with a long-term condition. Through this process parents developed a wealth of knowledge and expertise that could be further harnessed in the clinical interaction to improve outcomes for children and their families.
Interactions
The analysis highlighted that poor coordination and communication causes substantial frustration and distress, compromising trust in NHS staff members which can lead to poor health-care outcomes.
Parents described the essential role they play in ‘coordinating all the different appointments’ (P01), and expressed their worry that if they did not coordinate care, they were unsure who else would.
‘I just worry that some kids would fall through the cracks… it's not because they're not loved, it wouldn't be that but you know they might not have the capacity to be able to do that for their kids.’
P11
Parents wanted someone to integrate their child's care, resulting in less pressure on them to fulfil this role, as ‘it almost becomes a full-time job managing it’ (P01). The minority of families with an assigned paediatrician for this role, found this helpful.
The centrality of support
Parents described the centrality of support in their lives, and how this prevents feelings of isolation and enables coping. Such support is expansive and multifaceted, incorporating NHS staff, family, friends and others. Parents often experienced exceptional support from their respective clinical teams, particularly when the child had a condition such as diabetes or cystic fibrosis and were solely under one multi-disciplinary team. Parents reported accessing counselling or CBT, often through their GP, to support them.
‘I went to the doctors crying and I just said that I couldn't take anymore. So, it was actually the doctor that sorted it out for me.’
P03
Parents felt nursery or schooling was a form of respite for them during the day and enabled them to work. One parent described how ‘lockdown’ due to the COVID-19 pandemic highlighted the respite they get when their child is at a school which caters to her condition.
‘With this lockdown thing, it's just a bit more prevalent, everyday same routine, just shows how much they do at school with them, that we get to rest through the day.’
P15
Parents described friends and family as a crucial source of support. Peer support with other parents of children with similar conditions was described very positively.
‘The most information that I find out is from other parents.’
P12
However, some found this unhelpful, particularly when other parents manage the condition very differently. For example, one parent described how another ‘wraps her children in cotton wool’ (P04) and they would not manage their child in the same way. Many parents attended virtual support groups. However, some parents did not like to use them due to the wide differences between and within long-term conditions and because of the competitive nature of parents sharing their ‘war’ stories.
‘…what I find what it becomes is…which child is sicker competition… it almost ends up not being about support. It ends up being… I want to tell you my war story. I want everyone to try and better it… So, it ends up not being a support.’
P01
Such findings indicate a need for clinicians to understand the substantial challenges of impact and the necessity of support, and incorporate co-ordination of care and promotion of broader supports into their routine care.
Experience of care
This theme was universally commented upon by participants, particularly navigating the challenges associated with hospital appointments. Our findings indicate NHS appointment systems require improvement to reduce the negative impact on lives.
Appointments require substantial pre-planning and have repercussions on many areas of the parents' lives. This is summarised in Figure 2.
‘So, it's always a bigger deal than just going to an appointment…’
P02
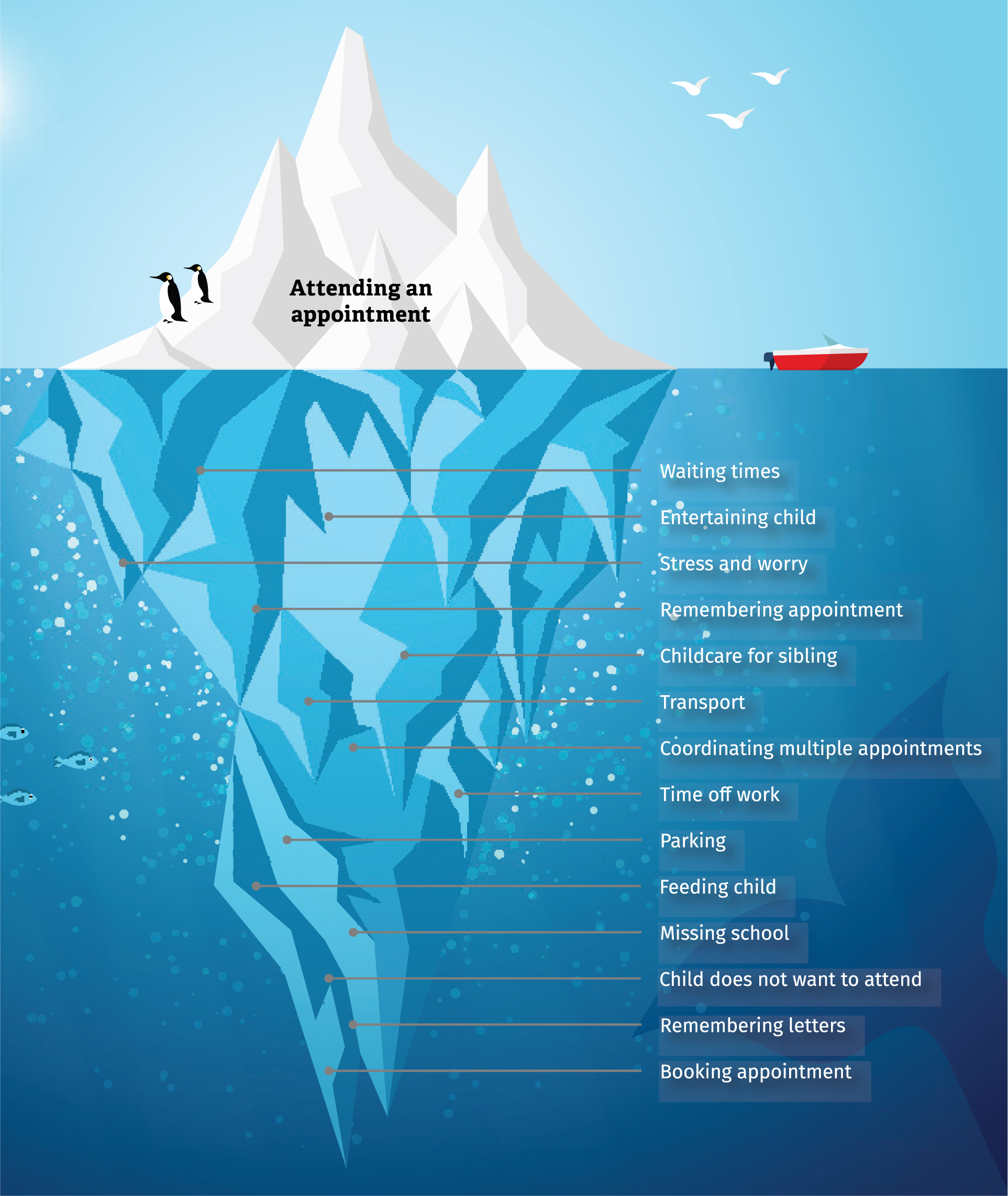
The difficulty of frequent appointments is made worse by poor coordination between clinics. Often, frequent appointments had a greater impact on their life than problems associated with the condition.
‘…it's been more of the, more of the appointments and all the kind of change to, like, daily schedules when appointments have come about, rather than his actual problem.’
P07
There is an associated negotiation for time off work for the parents to attend and an impact on the child's schooling and attendance. Alongside the practical planning, there is the stress of the experience due to long waiting times, resistance from children not wanting to attend and lack of car parking at hospitals, for example. This often meant parents are not in the right frame of mind to use the time effectively.
‘I've nearly missed appointments, it's so stressful and then by the time you get in you're not in the frame of mind to be able to list the concerns you had…’
P11
Our findings indicated many challenges were related to the NHS system rather than clinical care, which warrants further exploration of the use of remote consultation.
Discussion
This research has brought into focus the experiences of parents caring for children with long-term conditions and the substantial impact on parents and family life. This is a picture of complexity. The data indicates that parents have a wealth of knowledge about their child and the long-term conditions (Smith et al, 2015). This clarity enables health-care practitioners to understand the needs of parents and to consider how best to support them.
The vital role parents play in managing and coordinating their child's care led to feelings of overwhelming responsibility. This emphasises the importance of effective support systems for the whole family (Trollvik and Severinsson, 2004; Williams et al, 2007). The use of counselling and CBT by parents shows the value of talking therapies. Peer support can be useful, often when parents have formed these friendships themselves through support groups or previous encounters (Burke et al, 2018). Many of the parents found virtual support groups by chance and not from their clinical team (Smith et al, 2015). This research shows that advice on where to access support should be central in helping these families.
Effective communication between health care and parents made them feel more supported. Trust is compromised when parents experience conflicting communication about their child's care (Miller et al, 2009; Nygård and Clancy, 2018). Ensuring parents feel listened to is crucial as it leads to a cohesive relationship in which parents trust health-care professionals and feel they receive individualised care. This emphasises the importance of ‘family-centred care’ (Smith et al, 2014). Many parents wish there was a health-care professional whose role it is to integrate all of their child's care; those lucky enough to have this reported it worked effectively and felt supportive. Willis et al (2015) recommended that children with long-term conditions should have a ‘named’ GP to fulfil this role, but variability exists in operationalising this role.
This research highlighted the disconnect between services, leading to inefficient use of resources. Parents experienced issues with accessing appointments and report that discrepancies between services exist. Best practice should be shared between specialties and hospitals, initially outlined in the NHS LTP (NHS, 2019). This research highlighted in greater depth the organisation required for an appointment, including negotiation with employers. The representation of this in the ‘appointment iceberg’ shows a real need to change the way this service is provided in health care. The COVID-19 pandemic resulted in a forced move toward remote consultation, but may have just initiated a change which was inevitable. If parents had more choice in relation to appointments, then they could be used more effectively.
Strengths and limitations
This study explored the experience of parents of children with a range of physical long-term conditions. Having a range of long-term conditions was considered a strength as it allowed exploration of common themes appearing in a variety of conditions, improving transferability. The use of a stakeholder group to ensure PPI throughout the research was another important strength. The pathways for recruitment of parents were a limitation. Although two sources were used in an attempt to diversify the sample, one of the routes for recruitment was through the university volunteers' mailing list of staff. This will have reduced the diversity of the sample as they have a common employer, so may have distorted the themes of work and finances. However, the parents recruited had children who had not recently been diagnosed with their condition. The most recent was 18 months. This meant they had time to reflect, so were able to provide insightful descriptions of their experiences.
Conclusions
This research has revealed the substantial impact on parents' lives of having a child with an long-term condition. Each day is unpredictable and is filled with a range of emotions and complexity. Parents tend to accrue support from different sources. We advocate for health-care professionals' involvement to ensure families continue to function despite the daily challenges. These families interact significantly with health-care services, and have a wealth of lived experience, indicating this could further inform service provision and ultimately improve care for others.
The research reveals the burden imposed on families due to the NHS system of care (Figure 2). Radical change to the configuration of appointments in the NHS is unusual. However, this has been operationalised to great effect in the past year as a response to the COVID pandemic, during which the use of remote consultations has been widely adopted. From our findings, the benefits of remote consultation would mitigate some of the challenges parents experience around hospital appointments. In conclusion, we would strongly recommend that remote consultations become a permanent feature of clinical care for children with long-term conditions.
KEY POINTS
- Parents describe the psychosocial impact of having a child with a long-term condition, which can often be ‘ongoing and relentless’.
- The ‘appointment iceberg’ illustrates the difficulty of regular appointments for the family and signifies that changes are required in the delivery of this service.
- The varying avenues of support that parents draw from and the essential role they have is described by parents.
- There is a disconnect between services, seen in poor coordination and communication in health care, resulting in parents being relied upon to ensure consistency of care.
REFLECTIVE QUESTIONS
- How can the health-care system be adapted to suit the needs of children and families with long-term conditions?
- What are the pros and cons of offering the choice of face-to-face or virtual appointments to mitigate the effects of ‘the appointment iceberg’?
- What are the pros and cons of assigning a central health-care professional to each child with a long-term condition? For your service, who would that be?

