Measles, mumps and rubella (MMR) are infectious diseases that can lead to severe complications including disability or death (Demicheli et al, 2012). Measles in particular is a highly contagious viral disease affecting both children and adults (Public Health England (PHE), 2019a) with unvaccinated children under the age of 5 years being most at risk of harm because of their vulnerability (World Health Organization (WHO), 2020).
Prior to the introduction of the MMR vaccine in 1988 (PHE, 2019b), major outbreaks of measles were seen every few years, resulting in millions of deaths each year (WHO, 2020). Since the vaccine's introduction, death rates have declined; however, in 2018, measles surveillance saw a rising trend of cases across Europe and led to the UK losing its ‘measles free status’ in 2019 (WHO, 2019). According to Demicheli et al (2012), fatalities are more commonly seen in countries with higher levels of deprivation and less advanced healthcare systems; however, the risk remains in any country, regardless of wealth. MMR, like many other infectious diseases, are preventable with vaccination, a cost-effective method of protecting the public and preventing ill health. The childhood immunisation schedule recommends two doses of the MMR vaccine: the first at 12 months old and the second at 3–5 years old, to ensure that those with a poor response to the first vaccine achieve an adequate level of protection (PHE, 2019a; b). The current MMR vaccination uptake for first vaccines in under 5-year-olds is high at 94.5%; however, uptake of second doses has fallen to 86.8% and the negative effect of social media has been linked to non-acceptance of this vaccination (Nuffield Trust, 2021).
Astrup (2019) defines vaccine hesitancy as a reluctance or refusal to accept vaccination and described it as one of the top ten risks to global health and reports that some of this hesitancy is being promoted through social media. In more recent years, social media platforms have acted as a source of information about childhood vaccinations and both non-evidence-based advice and negative messages can easily be accessed, which may negatively influence a parent's view. Many parents report they have been exposed to anti-vaccination messages, which has contributed to fear of side effects (Astrup, 2019). However, there has been a positive movement from some social media organisations, such as Facebook, who have agreed to have better controls on content posted about vaccinations (Astrup, 2019). These platforms can also be beneficial and allow public health teams to target areas of poor uptake and promote helpful evidence-based advice on immunisations from a reliable source on a large scale. Jacobson Vann et al (2018) states that parents appreciate reminders from healthcare services about immunisations for their children and so, if used appropriately, adverts on social media may be helpful in achieving this.
It has been suggested that the fall in vaccination coverage may be a result of changes to the funding of public health services over the last decade (Nuffield Trust, 2015). For example, public health nurses who are overstretched because of budget cuts are less able to provide information to parents about vaccine safety. As research by Ames et al (2017) has shown, parents appreciate balanced information about the risks and benefits of a vaccine, in a timely manner, from a trusted healthcare professional, such as a health visitor. A reduction in this information can potentially lead to a lack of uptake. Parents who are well informed are more likely to believe that vaccinations are beneficial for promoting health (Wellcome, 2018).
 Well-informed parents are less likely to be vaccine hesitant, but a lack of money and resources for services may result in problems with healthcare professionals' ability to provide information on a vaccine's benefits
Well-informed parents are less likely to be vaccine hesitant, but a lack of money and resources for services may result in problems with healthcare professionals' ability to provide information on a vaccine's benefits
‘…parents appreciate balanced information about the risks and benefits of a vaccine, in a timely manner, from a trusted health professional, such as a health visitor.’
‘…higher levels of vaccination coverage are required to achieve herd immunity with diseases that are highly contagious…Hesitancy towards the [measles, mumps and rubella] vaccination therefore presents a major challenge’
For some parents, it could be the case that the perceived risks outweigh the benefits with regards to MMR vaccination. Despite the MMR vaccine being safely implemented in many countries worldwide, coverage fell from 90% to 80% between the late 1990s and early 2000s, because of findings published by a flawed, retracted study by Wakefield et al (1998), which linked the combined MMR vaccine with autism (PHE, 2019a). Despite a large body of evidence reporting that there is no confirmed link between the vaccine and autism (PHE, 2019a), or any of asthma, Crohn's Disease, leukaemia, gait disturbance, type 1 diabetes, hay fever or demyelinating diseases (Demicheli et al, 2012), parents continue to cite these as concerns in practice as reasons for their hesitancy.
Complacency of risk can be a factor for non-vaccination when a particular disease is very rare and/or the perceived risks are low (WHO, 2013). However, the reason for low prevalence of a virus is the result of continued delivery of vaccination programmes and sustainment of herd immunity. Overall, 95 out of every 100 children need to be considered immune to achieve herd immunity (Cockman et al, 2011). When herd immunity is achieved, there is enough protection within the community for the remaining 5% of the population to be protected against the disease, which benefits those who may be unable to have the vaccine because of risk of anaphylaxis or being immunocompromised. Sadarangani (2016) explains that higher levels of vaccination coverage are required to achieve herd immunity with diseases that are highly contagious, such as measles. Hesitancy towards the MMR vaccination therefore presents a major challenge to achieving protection at a community level.
Cultural differences and vaccine ingredients may also be a barrier to vaccination for some parents, although porcine gelatine-free vaccinations are available to accommodate religious practices in Muslim and Jewish communities (PHE, 2019a). A study carried out in the London borough of Tower Hamlets (Cockman et al, 2011) looked at first doses of MMR vaccines and found that herd immunity was possible in a lower income area with a high Islamic population. Uptake increased from 80% to 94% over a two-year period through the use of incentives, using technology creatively and gaining better understanding of the characteristics of hard-to-reach groups. This study by Cockman et al (2011) demonstrated that in the absence of compulsory vaccines and within areas of higher deprivation and ethnic diversity, vaccine hesitancy can be overcome by the impact of healthcare practitioners and their role in supporting parents to make an informed decision when choosing to vaccinate their children.
In the United Kingdom, it is not compulsory for children to be vaccinated and parents are required to make a choice about a vaccine, until their child reaches an age where they are deemed ‘Gillick competent’ and can consent for themselves. Targeting unimmunised teenagers who can self-consent could be a beneficial way of developing herd immunity within secondary school settings, as research by the Nuffield Trust (2021) suggests the 2018 measles outbreak was linked to unimmunised teenagers. The school nursing service can help to raise awareness of MMR and encourage vaccination uptake. In Italy, a country where measles transmission rates are higher than the UK (Oxford Vaccine Group, 2019) initiation of compulsory vaccines for school entry has been trialled. Trentini et al (2019) gathered positive results on compulsory vaccination and for some parents, this strategy may be a motivating factor, as parents will be required to prioritise vaccinations before their child starts school. Compulsory vaccines, however, may lead to psychological resistance in parents and could be viewed as coercive, taking away their right to choose (Miller et al, 2007), which may further exacerbate negativity towards vaccinations (Astrup, 2019).
Methods
The Joanna Briggs Institute (JBI, 2019) qualitative framework assisted the formulation of the research question, which seeks to explore a concept rather than to assess the effectiveness of an intervention. This review set out to analyse literature on parents' views around MMR vaccination and gain a deeper understanding about parent's health choices for their child.
A previous systematic review on parental decision making around MMR vaccinations was carried out by Allan and Harden (2015) using qualitative studies; however, this research is now dated and therefore it is beneficial to revisit this area. A recommendation was made by Allan and Harden (2015) for further research to examine factors that lead to a parent's choice to either consent or refuse the vaccine. Since then, a systematic review on childhood vaccinations was published by Ames et al (2017). This review focused on parental views about communication around childhood vaccination, including the MMR. Studies included in this Cochrane review were published prior to 30 August 2016, and therefore it was deemed appropriate for the present study to include research published from September 2016.
The JBI (2019) recommend the Population, Exposure, Outcome (PEO) framework, which is documented in Table 1, and resulted in the research question: What factors influence vaccine hesitancy amongst parents with regards to MMR vaccinations?
Table 1. Population Exposure Outcome framework
| Population | Exposure | Outcome |
|---|---|---|
| Parent* | MMR vaccin* | Vaccine hesistanc* |
| Care* | Measles vaccin* | Vaccine refusal |
| Guardian | Measles, mumps and rubella vaccin* | |
| Mother | ||
| Father |
Three databases were used in this review: CINHAL, MEDLINE and OVID. The initial search was carried out in November 2019 and was repeated in February 2020 to ensure the research included was as up to date as possible. Evidence was also retrieved by hand searching reference lists and journals, along with recommendations from experts in the field. The inclusion criteria were: primary research from academic journals, relating to MMR vaccination or to parents' decision to vaccinate their children or vaccine hesitancy.
The systematic review process is outlined in the PRISMA flow chart (Figure 1), which displays how the quantity of evidence was funnelled and filtered down to the number of results relevant to the research question.
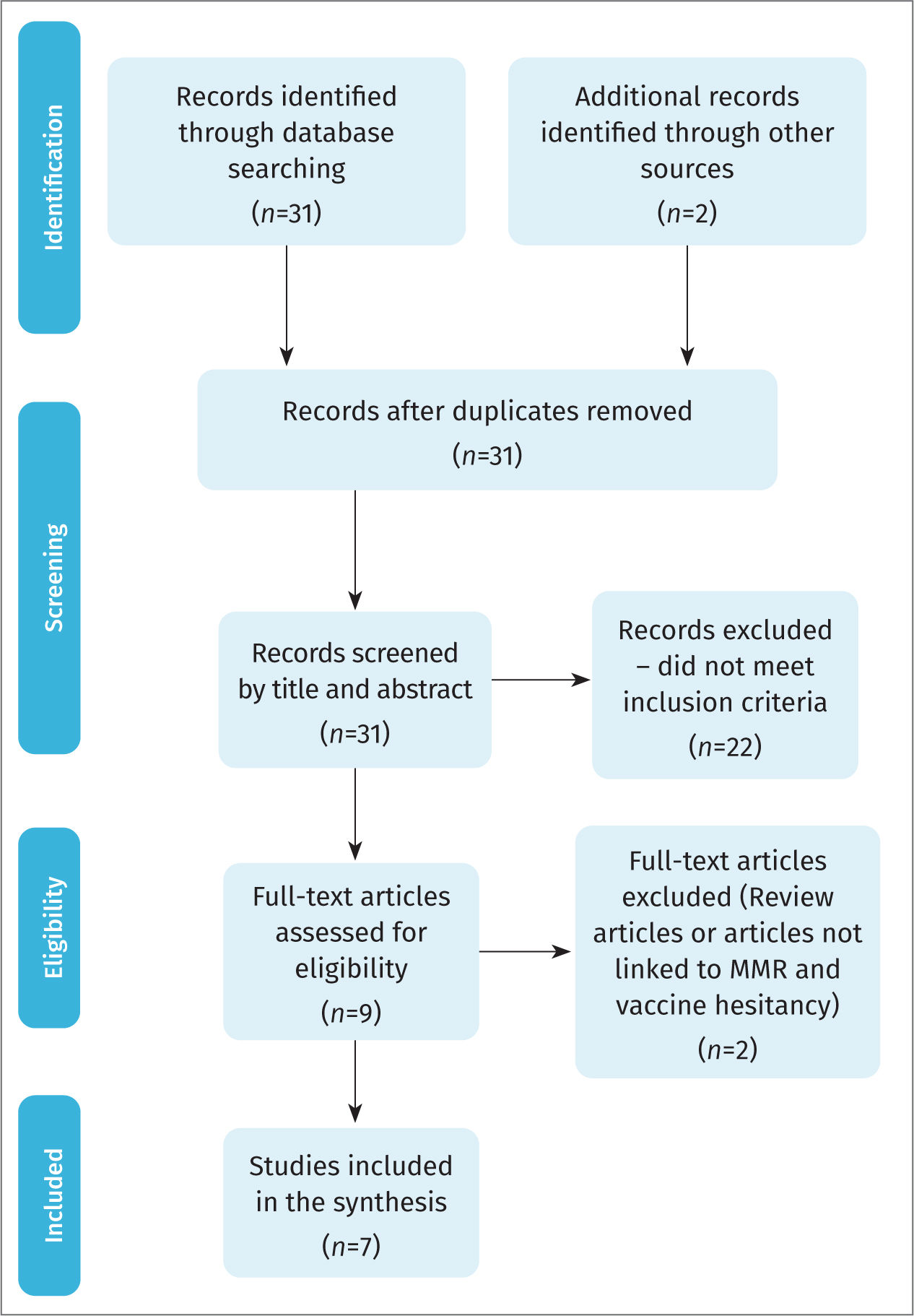 Figure 1. PRISMA flowchart
Figure 1. PRISMA flowchart
Seven studies met the inclusion criteria and are summarised in Table 2. Several critical appraisal tools were selected for this review, as appropriate to the individual study designs, including checklists published by CASP and the Joanna Briggs Institute (JBI). The critical appraisal tool used for each study is cited in Table 2.
Table 2. Details of studies included in literature review
| Study details | Aim | Methods | Results | Limitations |
|---|---|---|---|---|
| Helps et al (2019) Understanding non-vaccinating parents' views to inform and improve clinical encounters: a qualitative study in an Australian community. | Explore reasons behind vaccine refusal. | Purposive sample, 32 semi-structured face-to-face interviews with parents. Snowballing recruitment. Thematic analysis focused on parent's decision making and choice not to vaccinate. | Personal experience caused doubt about safety and concerns regarding consent gathering. Interactions with healthcare professionals could be dismissive and hindering, or helpful. Inflexibilities within healthcare service. Parents were on a quest for the ‘real truth’. | Interviews carried out in population with emphasis on natural health, not representative of wider Australian community. |
| Carpiano et al (2019) Socioeconomic status differences in parental immunisation attitudes and child immunization in Canada: Findings from the 2013 Childhood National Immunisation Coverage Survey. | Examine family socioeconomic status determining parents' knowledge, attitudes and beliefs on child vaccination. | Cross-sectional. Sample taken from data collected by Canadian Childhood National Immunisation Survey, included 24 853 girls aged 2–17 years. Random sampling of participants, stratified by geography. | 7% (2-year-old children): no vaccine, linked to safety concerns and lack of perceived importance. Knowledge attitudes and beliefs linked to non-receipt of vaccine in parents with negative views. Socioeconomic status inconsistently associated with knowledge, attitudes and beliefs and vaccine hesitancy. Lower socioeconomic status means side effects and safety concern more likely. Parents may require more mediation if less educated. | Design limits causal conclusions as study did not measure vaccine uptake over time. Outcomes may be out of date. |
| Moyer-Guse et al (2018) The Role of Humour in Messaging about the MMR vaccine USA. | Investigate influence of satirical message about the measles, mumps, rubella vaccine on resistance and hesitancy. | Randomised controlled trial of 187 parents of young children with at least one child under 9 years old. Parents randomly assigned to humorous message or serious message. | Participants in humorous group: less psychological reactance than non-humorous group. Greater reactance: greater vaccine hesitancy. Humorous messages: positive effect on those with increased false beliefs about vaccine. Humor not beneficial for parents with positive views. | Differences in humour. Measured attitudes not uptake. Method of randomisation not specified, concealment of allocation not stated. |
| Perinet et al (2018) Delayed measles vaccination of toddlers in Canada: Associated socio-demographic factors and parental knowledge, attitudes and beliefs. | Examine delays with first MMR vaccination in relation to parents' socioeconomic status, knowledge attitudes and beliefs. | Information from 2013 survey with 3604 children. Stratified sampling based on age of child and geographic location. Parents asked for child's immunisation record and set of questions on socioeconomic status and knowledge, attitudes and beliefs. | 69% children given first vaccine on time. Delay more common in girls, and those born outside Canada. Children in single parent households: longer delay for measles, mumps and rubella uptake. Vaccine hesitancy linked with delay, uptake increased over time. Delays linked to safety concerns had strongest association. Parents who value homeopathy significantly associated with delay. | No immunisation dates for over half of children. Only English or French speakers included. Lack of statistical power. Strongest associations did not reach statistical significance. |
| Machekanyanga et al (2017) Qualitative Assessment of Vaccination Hesitancy Among Members of the Apostolic Church of Zimbabwe: A Case Study | Collect views on vaccination from parents, religious leaders and healthcare professionals and explore factors associated with vaccine hesitancy. | Case study: 10 Apostolic parents of children aged 9–59 months, 90 parents, 60 healthcare workers and 10 religious leaders. Semi-structured interviews with religious leaders and key informants; structured interviews with Apostolic parents; focus group discussions with healthcare professionals. | Poor knowledge of vaccines and negative perceptions contribute to vaccine hesitancy, as do low levels of education, lack of understanding and appreciation of effectiveness of vaccine and religious teaching that emphasises prayers over medicine. Parents fearful of sanctions from religious leaders. Government should increase targeted efforts to address vaccine hesitancy within Apostolic church community in Zimbabwe. | Only some religious leaders agreed to be interviewed; the views collected may not reflect the wider Apostolic leadership in this area. |
| Gerede et al (2017) How to Increase Vaccination Acceptance Among Apostolic Communities: Quantitative Results from an Assessment in Three Provinces in Zimbabwe | Assess knowledge, attitudes and practices among Apostolic caregivers. | Purposive sample including Apostolic populations. Households selected at random. Questionnaires made following discussion with immunisation programme officers who work with Apostolic communities. Structured interviews carried out with 97 caregivers from Apostolic community. Vaccination status collected for 126 children aged 9–59 months. | 30/126 children been vaccinated, 73% of caregivers with unvaccinated children held very strong beliefs, would never vaccinate their children. Mothers in monogamous relationships more likely to have antenatal contact (where immunisations are discussed). Parents less well educated, more likely to be unemployed. 42% were Johanne Marange, who are less likely to immunise. 57% would be happy to receive information about childhood vaccinations and would prefer it came from a nurse or health worker. | No comparison of non-Apostolic groups. Sample size too small for statistical analysis of subgroups. Extraneous variables not explicitly mentioned: poor record keeping around childhood immunisations is a concern. |
| Palanisamy et al (2018) Social Capital, trust in health information and acceptance of Measles-Rubella vaccination campaign in Tamil Nadu: A case-control study | Assess influence of social capital and trust in health information on measles-rubella vaccination campaign. | Case control study of two groups of children aged 9 months to 15 years, with parents who refused vaccine (92 cases) and children who received it (92 controls). Four villages selected randomly. Groups completed two questionnaires: social capital scale and vaccine hesitancy scale. Questions also measured views on trust in sources of health information. | Younger parents more likely to refuse vaccine. Vaccine acceptance greater when offered at school. Parents who trusted school teachers more likely to accept vaccination. Those with older children and greater trust in health information more likely to accept vaccination. Child's age, parental attitude toward vaccination and trust in health information provided by school positively influenced uptake of vaccination. | Sample size small although proportional to village size. Selection of participants was non-random, based on convenience. Other factors not assessed may influence decision to vaccinate. |
The findings of the studies were combined, grouped into key themes and coded by hand as part of a thematic analysis (JBI, 2019).
Results
Thematic synthesis resulted in five themes emerging from the studies, which are outlined in Table 3.
Table 3. Key themes
| Theme | Author(s) |
|---|---|
| Parental knowledge, attitudes and beliefs | Carpiano et al (2019) Moyer-Guse (2018) Machekanyanga et al (2017) Gerede et al (2017) Palanisamy et al (2017)Perinet (2018) |
| Socioeconomic status and vaccine hesitancy | Carpiano et al (2019) Perinet (2018) Gerede et al (2017) |
| Parental concern regarding vaccine safety | Helps et al (2019) Carpiano et al (2019) Perinet (2018) |
| Provision of information | Palanisamy et al (2017)Gerede et al (2017)Moyer-Guse (2018) |
| Views on natural health and lifestyle | Helps et al (2019) Perinet (2018) |
Parental knowledge, attitudes and beliefs
Vaccine hesitance is associated with a parents' knowledge, attitudes and beliefs. This was the strongest theme and was identified in the majority of studies (Carpiano et al, 2019; Moyer-Guse et al, 2018; Machekanyanga et al, 2017; Gerede et al, 2017; Palanisamy et al, 2018; Perinet et al, 2018).
Palanisamy et al (2018) identified that parents who are well bonded to their community, are likely to engage with the beliefs of that community, whether positive or negative. Therefore, if MMR vaccinations are trusted within a community, parents who are well connected socially are more likely to vaccinate their children. Tamil Nadu is an area where poor uptake of immunisation is common and parents who have high social capital and stronger links with their community have been found to be less likely to agree to vaccination. Palanisamy et al (2018) carried out a t-test to compare the mean score of parents' attitudes towards vaccination from the vaccine hesitancy scale. Parents were more likely to accept vaccination if it was offered at school (P=0.000) and if they trusted schoolteachers (P= 0.003)
Carpiano et al (2019) concluded that knowledge, attitudes and beliefs were linked to non-receipt of MMR vaccination in parents who viewed the vaccine to be unimportant. Ambivalence towards vaccination was linked to lack of education, which is reflected by Perinet et al (2018). Perinet et al (2018) carried out logistic regression to assess the association between positive vaccine uptake and parents who were knowledgeable about childhood vaccination. The author identified that vaccination was most commonly delayed by 1–6 months if parents believed the vaccine was unsafe. However, the data were only collected from parents who could respond in English or French, so the results are not truly representative of the cohort of Canadian children in this age group.
Gerede et al (2017) selected a purposive sample, which is beneficial when investigating a targeted group or community. Households within Apostolic communities in Zimbabwe were selected at random and semi-structured interviews with parents were used to gather information from participants. Only 30 out of 126 children had ever been vaccinated and 73% of caregivers with unvaccinated children were reported to have very strong beliefs, stating they would never vaccinate their children.
Machekanyanga et al (2017) carried out a qualitative study focused on perceptions of community members within the Apostolic community. Healthcare workers viewed poor knowledge of vaccines and negative perceptions around vaccination to be the main factors contributing to vaccine hesitancy. Semi-structured interviews and focus groups were organised to gather views and opinions about factors contributing to vaccine avoidance. Healthcare workers and public health teams who took part in the study identified how religious teachings that emphasise the benefits of prayer and holy water over the use of medicine can cause hesitancy. The fear of religious sanctions for a parent who allowed their child to be vaccinated further exacerbates this hesitancy. This study was carried out in a very niche population; however, it does enable a deeper understanding of cultural factors that may contribute to a parent's decision about whether to vaccinate.
Socioeconomic status and vaccine hesitancy
Carpiano et al (2019), Perinet et al (2018) and Gerede et al (2017) conclude that there is a link between lower socioeconomic status and vaccine hesitancy, with regards to some specific vaccinations, such as MMR. Carpiano et al (2019) and Perinet et al (2018) used information from the same dataset, collected in 2013 by the Canadian Childhood National Immunisation Survey, which is carried out every two years and provides a sampling frame based upon the Canadian child tax benefit list. A limitation of the sampling frame is that this does not include the whole population and many families with immigrant status and very low socioeconomic status could have been excluded.
Perinet et al (2018) examined vaccination delays of the first MMR vaccination in children aged between 12 and 30 months. Children living in single parent households were more likely to have longer delays regarding MMR uptake and delays were more common in girls and those born outside of Canada. However, vaccination uptake was reported to increase over time. Carpiano et al (2019) responded to the findings of Perinet et al (2018) and used the same dataset to further investigate the girls within the cohort and observed an inconsistent link between socioeconomic status and safety concerns. The authors reported that parental concerns were vaccine specific, rather than being related to all childhood vaccinations. Parents were found to have less confidence in the MMR vaccine and were more likely to feel concerned about the safety of the vaccine if they had not been educated at a university level (Carpiano et al, 2019).
Gerede et al (2017) interviewed 97 caregivers and also identified that parents in the Apostolic geographic cluster of undervaccination, had received less formal education and were more likely to be unemployed.
Parental concern regarding vaccine safety
Many parents are concerned about the possible side effects of the MMR vaccine (Helps et al, 2019; Carpiano et al, 2019; Perinet et al, 2018). Perinet et al (2018) discovered that vaccination delay was linked to concerns over vaccination safety and this was found to be the most statistically significant finding for parents who had 2-year-old children of both sexes. Safety concerns relating to MMR vaccination were linked to delays of 7–18 months. Carpiano et al (2019) further found most parents had received contact from a healthcare provider prior to receipt of the vaccination, which indicates that the contact provided a stimulus for the uptake of the vaccine.
Helps et al (2019) selected a purposive sample to gather views of parents within an Australian community that had high rates of vaccine refusal. Participants were recruited via a snowballing approach, which was helpful in accessing harder to reach parents who would not otherwise have agreed to take part in the study. Semi-structured interviews took place and Helps et al (2019) found that 24 out of 32 parents recalled a negative personal experience of someone becoming unwell following a vaccine, causing them to doubt the safety of a vaccination, which in turn led to avoidance or refusal.
‘…teachers played an important role in influencing parents to have their child vaccinated with [measles, mumps and rubella] vaccines, and vaccine acceptance was found to be higher if provided at school.’
Views on natural health and lifestyle
Helps et al (2019) and Perinet et al (2018) agree that parents who value natural health and lifestyle are less likely to consent to childhood vaccinations. Perinet et al (2018) found a strong association (odds ratio 3.60) between vaccine delays of 7–18 months in children whose parents believed in alternative medicine. Parents who felt natural lifestyles could replace vaccinations were three times as likely to delay measles vaccines, compared to parents who did not report valuing natural health over medical healthcare (Perinet et al, 2018).
Helps et al (2019) explored parents decision making processes around vaccinations in a community that had a strong emphasis on natural health remedies and lifestyle. Results indicated that participants held neutral views around vaccinations prior to becoming parents; however, they also reported experiencing events that led them to question the benefits of childhood vaccination. Only two out of 32 parents referred to having an intuitive desire not to vaccinate their children and for most parents, the decision not to vaccinate was said to be a difficult one.
Provision of health information
Palanisamy et al (2018) and Gerede et al (2017) found parents appreciate information about childhood vaccination from others in professional positions and view teachers and healthcare professionals as trusted sources of information. Palanisamy et al (2018) found that teachers played an important role in influencing parents to have their child vaccinated with MMR vaccines and vaccine acceptance was found to be higher if provided at school. This finding is supported by Gerede et al (2017) who found 57% of respondents within the community, where undervaccination is prevalent, stated they would accept information about vaccination and 66% of these responders stated a preference for information to be provided by a healthcare professional. Gerede et al (2017) also found that a small percentage of caregivers suggested it might be helpful to engage church leaders with vaccination campaigns.
Palanisamy et al (2018) carried out a case control study, which found that parents who were more trusting of health information were more likely to accept the MMR vaccine. However, the authors stated that the findings were based on a small sample size (184), which limited the statistical power of the results. Palanisamy et al (2018) also found that acceptance of the vaccine was lower among parents who trusted social media as sources of vaccine-related information. The study identifies an association between younger parents and non-uptake of the MMR vaccination. They concluded that it was more likely that younger parents use social media as sources of health advice and consequently, are at a higher risk of being misinformed about vaccine safety and benefits.
It may be the style of social media messages that parents find engaging, as Moyer-Guse (2018) found that parents who receive information about MMR vaccinations in a humorous way were less vaccine hesitant.
Discussion
This systematic review indicated that the strongest factor for vaccine hesitancy towards the MMR vaccine was linked to the knowledge, attitudes and beliefs of parents. This theme was supported by six out of the seven studies and has been defined as the overarching theme of the review. Although the knowledge, attitudes and beliefs of parents was the strongest finding of the review, there are many factors that contribute to vaccine hesitancy amongst parents and inform their knowledge, attitudes and beliefs.
After parents' knowledge, attitudes and beliefs, socioeconomic status and concerns around vaccine safety were strong influencing factors. Higher levels of formal education appeared to result in increased knowledge and understanding of how vaccines work in a helpful way to protect the health of a child as well as the wider community. A good knowledge base such as this allowed parents to dispel myths around safety, with the support of the healthcare system and enabled them to make an informed choice, which resulted in vaccination for their children.
Perinet et al (2018) observed a strong association between parental safety concerns and vaccination delays of up to 6 months, which leaves children vulnerable during this period of delay. Safety concerns may be associated with certain vaccinations, such as MMR, which are known to carry more negative connotations amongst parents. Although the majority of parents are accepting of the MMR vaccination even if they delay uptake, there are certain groups of parents who avoid the vaccines and some of these groups have been explored in this review. MMR vaccination delays were observed by Perinet et al (2018) in single parent households, where there might be additional barriers that may impact on a parent's ability to prioritise vaccination appointments. Perinet et al (2018) also found MMR delays in children born outside of the country they reside in, which may be the result of variations in immunisation schedules from country to country. Parents who face language barriers could also experience difficulty accessing appropriate information and difficulty arranging appointments, emphasising the importance of interpreting services, as well as the influence of the lower socioeconomic status that migrant families often face.
A parent's decision-making process with regards to childhood vaccination is complex, with many reasons why a parent might choose to delay or refuse to vaccinate their child against MMR. It appears that the decision is influenced by several factors, rather than one individual reason. The decision may be the result of a negative experience in the past, where they knew of someone who developed side effects following vaccination (Helps et al, 2019). This could be followed by an interaction with a healthcare professional who did not alleviate their concerns and, as a result, parents seek out information from other sources, such as the internet, which can provide conflicting or negative advice. The WHO (2012) constructed guidance for healthcare professionals on how to talk to parents about vaccination, which was published in 2012. This guidance offers practical advice for healthcare practitioners on how to offer reassurance to parents about the risk of vaccine side effects.
Ames et al (2017) concluded that parents wanted to receive more information about childhood vaccinations and viewed healthcare professionals as a helpful resource. Ames et al (2017) also identified a need for more research to be carried out on childhood vaccination in rural, low-and middle-income countries. Therefore, it was beneficial to include a range of countries in this systematic review. This systematic review included studies from Africa, India and rural Australian communities, and highlights some of the variations in the values and beliefs of parents with regards to methods of preventing ill health. Community and religion can have a strong influence on a parent's decision to vaccinate and Gerede et al (2017) reported that some parents suggested home visits may be beneficial in communities where vaccination is more controversial. This systematic review finds that in general, parents are happy to receive information about vaccination from trusted professionals, such as schoolteachers and healthcare professionals, and includes the views of parents from rural communities where immunisation uptake is less common. Previous research carried out by Saeterdal et al (2014) also supports the view that involving religious leaders is helpful in promoting vaccination uptake.
‘Community and religion can have a strong influence on a parent's decision to vaccinate…some parents suggested that home visits may be beneficial in communities where vaccination is more controversial’
Not only do parents base the decision to vaccinate on their own knowledge, attitudes and beliefs but also on those of their community (Palanisamy et al, 2018). However, this can cause unnecessary avoidance of vaccination and can lead to the formation of geographic clusters of non-vaccination. The study carried out by Cockman et al (2011) in the London borough of Tower Hamlets demonstrates that professionals can successfully increase vaccine uptake in communities with higher levels of deprivation and minority ethnic groups through a range of interventions.
Perinet et al (2018) found a strong association between homeopathy and vaccine hesitancy, compared to vaccine safety. Helps et al (2019) interviewed parents from a community where natural lifestyles are prominent and found that parents reported that safety was their main concern, as they wanted to avoid any harm coming to their children. This resulted in parents experiencing internal conflict around whether to vaccinate their children (Helps et al, 2019). Although some natural medicines have been claimed to prevent or treat childhood illnesses such as measles, there is no evidence to support this as an alternative to traditional immunisation (National Centre for Immunisation Research and Surveillance, 2014) and consequently healthcare professionals must increase their efforts to share this knowledge and promote vaccinations.
As a result of the COVID-19 outbreak, some parents have avoided taking their children for routine vaccinations, such as measles, because of fear of coming into contact with the virus, along with government instruction to stay at home. Despite this and according to the Nuffield Trust (2021), the national lockdown measures have led to a reduction of reported cases of measles. Therefore this may be an opportune time in the campaign to increase the uptake of the MMR vaccine.
This review has highlighted that there is a lack of recent qualitative research on MMR and vaccine hesitancy. Further qualitative research on this topic would be beneficial, given that parental concerns about safety are still so prevalent across the world and have contributed to the UK losing its ‘measles free status’. The review also identified a lack of up-to-date UK-based research. Consequently, the results of the studies presented are less applicable to UK populations. Several studies included in this study investigated niche populations, which is useful as there has been a reported gap in the literature related to low- and middle-income countries. A limitation of this review is that the studies included were not carried out in the UK; however, they do provide insight into vaccine hesitancy around MMR from a range of cultures and communities, which may be useful when working in areas of rich diversity within the UK.
Conclusions
In conclusion, the findings from this systematic review highlight that a parent's knowledge, attitudes and beliefs are the main factor associated with vaccine hesitancy and decision making around MMR vaccinations. The topic is complex in nature and it is helpful to understand that there are several factors that influence a parent's decision to consent to MMR vaccinations and to be aware of these factors for their potential to lead to non-vaccination. Although the majority of parents do consent to MMR vaccination in the UK, there are some groups where vaccination uptake is less common and overall vaccine hesitancy is preventing herd immunity from being achieved. Ongoing efforts and health promotion can promote better insight and positive attitudes towards MMR vaccination. These efforts will support the UK to work towards regaining its ‘measles free status’.
KEY POINTS
- More can be done to provide parents with trusted sources of information.
- Additional efforts are needed to increase parent's knowledge and could be used to assist future planning of MMR vaccination delivery.
- Multiple factors are associated with vaccine hesitancy or delay including, parents with poor health literacy, from certain religious groups, migrant populations, and low socioeconomic backgrounds.
- In areas where there are high concentrations of such groups, parents may need additional information and support from healthcare professionals.
- It is important for healthcare professionals to discuss immunisations with parents, offering time to share evidence and alleviate concerns about vaccine safety with a view to making each contact count.
- Parents are more comfortable with the idea of vaccinations if the child's school is supportive of the vaccination.
- A whole community approach to encouraging MMR vaccination should be taken, including offering information to parents at community events, through school assemblies or parent evenings, liaising with religious leaders, children's centre staff, GP surgeries and the addition of health promoting messages about childhood vaccinations on the school health screening questionnaire.
REFLECTIVE QUESTIONS
- Do you know what the MMR uptake is in your area? Would it provide herd immunity to the population?
- What are the views of parents with regards to MMR vaccination in your practice setting?
- Routine childhood vaccinations have been available during the pandemic, however some parents may have been fearful of taking their child into the GP surgery. Are there children on your caseload who may have outstanding immunisations for this reason?
- In the current climate, what would you say to a parent to reassure them that MMR vaccinations are safe and effective?

